We’d love to share a little more about our company and our solutions.
Download for more details on what we do and who we serve. Contact us with any additional questions – we’re here to help!
Open me
Need formal reporting, at scale?
Need interactive dashboards with data visualizations?
Need to present analytics alongside original content or commentary?
Learn more
SDoH analytics requires a lot of data, and different types of data. Claims data tells us about health care visits. Digital device data tells us about daily health. And special data sets let us delineate the social and environmental factors that could influence each member.
In SDoH analytics, we understand each person as an individual and in context, but look at a community as a whole in aggregate, to see what trends and patterns emerge.

Here are 5 important aspects to consider, and tips of what to look for, so you can trust the insights in your SDoH analytic endeavors.
Wellness means care and lifestyle choices. This data is scattered across many different places. Health analytics must integrate complex claims data structures and lifestyle data at an individual person level. SDoH analytics should also be connected at a person level. This way, the data is ready to serve all the analytic questions you may ask, without additional data preparation and delays.

The more granular a data set is, and assuming it is associated at a member-specific level, the more trustworthy and usable your SDoH insights will be. Think about the variation of social and environmental factors you see across an entire zip code. Now think about the degree of variation you see within a neighborhood. A Census Block Group is akin to a neighborhood. This means if you have source data that has a Census Block Group level of granularity, you are seeing only the degree of variation across neighborhoods, not entire zip codes.

Social and environmental factors cover a broad range of influences on health. Air quality or water quality? Economic hardship or transportation access? There is so much we can do if we have lots of different SDoH indices to choose from. For instance, one HDMS client is looing at the transporation index alongside the technology index to assess the potential usefulness and impact of a mobile unit verse a virtual solution for specific care services. Locations with low transporation AND low technology indices are prioritized for mobile services, while other locations are suitable for virtual care alternatives.

HDMS offers over 25 SDoH indices and dimensions.
Start with composite indices that allow you to look broadly across a number of factors at once. Use focused indices to support very specific or nuanced investigations, like food access or social isolation. They can also be used together – for instance the transportation index and the technology index example we shared above.
Have a good understanding of which social or environmental factor you are investigating and where that index is sourced. There are a wide variety of options. Nothing will be perfect. Some indices are more complete, more granular, more recently or frequently updated, than others. As you interpret results, have transparency around the process leading to the metrics. This will help everyone interpret and apply insights better in the long run.

TIP: Enriching claim data delivers fast and intuitive investigations. This makes SDoH analytics easier too.
Enrichment can have many forms: classify claims by episode treatment groups (ETG), apply pharmaceutical classifications, and flag specialty druges. Enrichment processing also identifies gaps in care and low value care and makes it easy to surface these individual moments into analytics.
ER visits that have been classified using the NYU methodology allow you to quickly look at who visited the ER for non-emergent care, just by using a few filters. Now think how powerful it is to further see these visits by income index.
As we think about integrating new data to investigate social determinants of health, we naturally focus on the new data – the addition. But we need to link that to core health data. Let’s not forget the quality and usability of those systems or sources. The data quality processes surrounding your traditional analytics are a critical part of trusted SDoH insights.

HDMS Enlight offers the most comprehensive out of the box SDoH analytics on the market.
Explore SDoH Analytics Contact us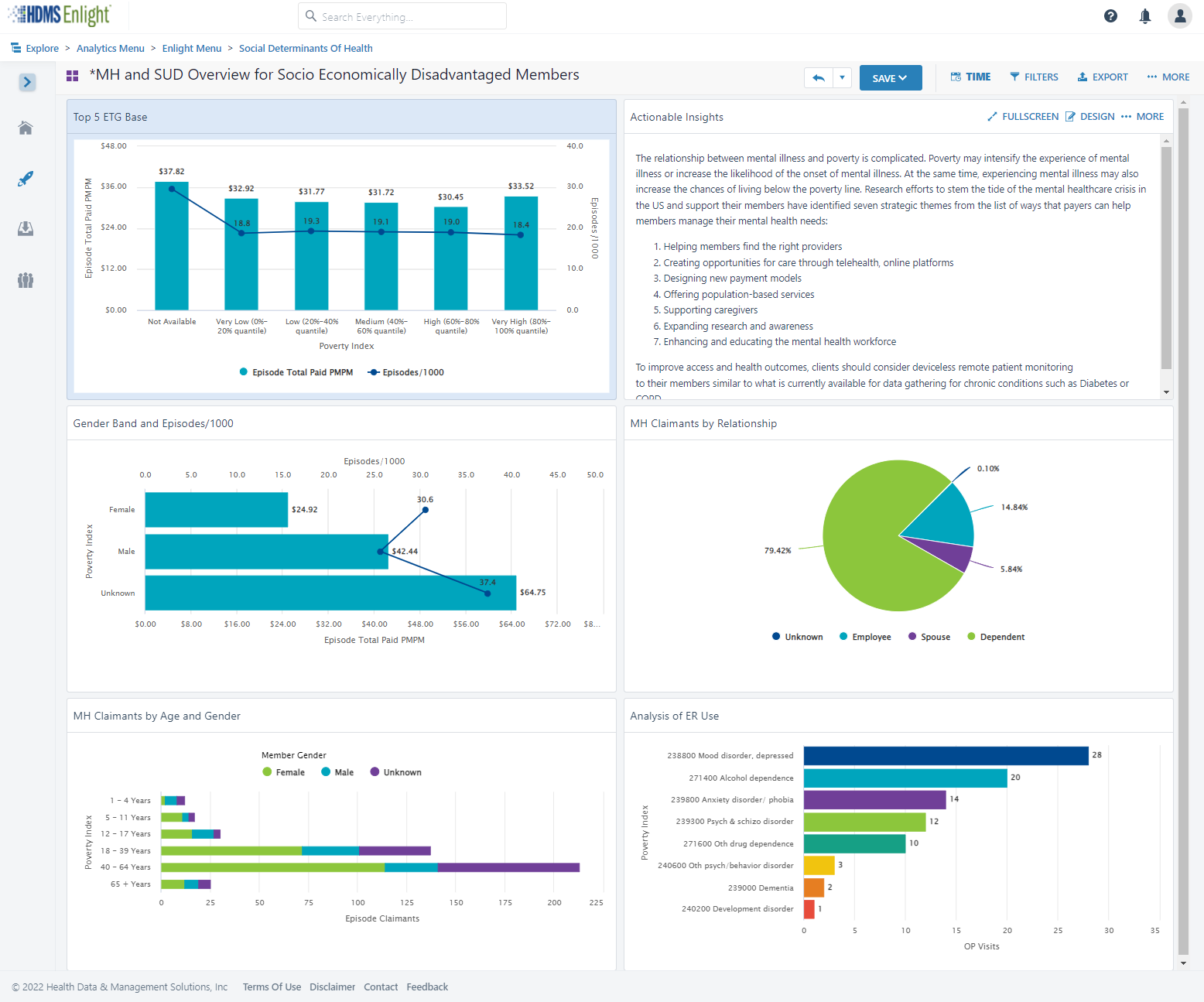
Did you ever have a home improvement project that finished late and cost more than you expected?
How about a technology implementation that finished late and cost more?

You are more likely to be on-time and on-budget if your plan is thoughtful and reflects your reality. Have confidence and know what you’re really getting into! Health data is very complex.
One-size does not fit all. It’s unlikely your implementation is the same as other organizations. Why?
Dig in. What are the details behind YOUR implementation plan?

Discuss what will be problematic or painful based on your experience and what you are moving away from. Are those complexities appropriately addressed, cared for, or resourced? Think about metric definitions and consensus, data quality, data reconciliation, matching and integration across sources, and slowly changing history.

Identify what is- and is-not in your control. If something is beyond your direct control, is there a named resource and escalation path? What risk does that pose to the project timeline based its nature. For instance, your health analytics implementation is reliant on data from others. How are your relationships and service level agreements with those partners and vendors? How does that affect your plan and what’s the back-up plan?
Before your implementation starts, refresh your knowledge of the day-to-day contacts, authorities, and any contractual SLA’s you have in place. If there will be costs associated with establishing new feeds or data interfaces, identify those early.
Top down, bottom up, or an interesting mix? Think about the approach that will work better for your organization. What process works for you – here’s my data – what can I do with it? Or here are my objectives – what data do I need? There are pros and cons to each but thinking about this as you prioritize is invaluable for setting internal expectations and getting the right resources lined up.

Use phase 1 for quick wins. Standard sources generally seamlessly populate the most common views. Users feel like they get a lot out of the gate and that helps tremendously with adoption.
Remember, you’re better off with an implementation plan that’s realistic rather than one that sounds like a dream but doesn’t work well for you in the end.
Learn about Enlight What is it like working with HDMS?
HDMS provides predicitive models, pre-defined segments, model scores, historical predictions and more.
Bring member-level scores and cohorts into a cross-prediction analytic view.
There’s power and sophistication wrapped up in an intuitive user experience – so you can do more than look back on historical trends.
Learn more
HDMS clients – have your team walk you through the latest models.
What do you do next? We’ll make sure your data supports your next steps and actions.

Every organization is different. Some are understaffed. Some handle everything in-house, some work with multiple trusted partners.
HDMS teams work around a collaborative Analytics Agenda. No matter who is a part of analytic work, we see how our work comes together and we progress results fluidly.
See a short video
It’s our way of making sure we understand your organization’s goals, culture, available resources and partners to create and use healthcare analytics for the benefit of your business and employee health. An Analytics Agenda is a documented plan that gives you clarity on how HDMS will make you successful.
We use Analytics Agendas to generate results momentum. That means not only do the reports and KPI dashboards you implement in phase 1 continue to deliver value, but we use the Analytics Agenda to find new ways and deliver new incremental value over time.
Help your organization grow – step by step, constantly moving the ball forward. An HDMS Analytics Agenda serves as a documented understanding of what your organization is trying to achieve, how healthcare analytics support priorities, and then digs into the tactical and technical aspects of what and how a collaborative team will perform work to deliver value in these spaces. Analytic efforts often focus across
Identifying where time is spent, what analytics are needed, and how data supports these efforts are all part of creating an Analytics Agenda.
Clients find creating this deliverable energizing because through the process we are able to formulate a plan that was otherwise difficult to progress internally. We guide you through this process so that you can lead within your organization. As creative problem solvers we are used to overcoming internal obstacles and we bring these strategies and ideas to your experience when you need help.
As the path and plan forward solidify, it’s time to get to work! Our Data Operations team handles the administration and execution of gathering data from your various data vendors. They carefully define data integration and data quality processes to deliver things like whole health views, total cost of care analysis, and high impact opportunities – based on priorities set in the Analytics Agenda.
We pull in early insights to refine the Analytics Agenda, considering both your analytic results as well as our collective intelligence of other organizations like yours. For instance, we might accelerate some tasks if we see an opportunity to reveal cost trend drivers that could be positively impacted if deeper analysis were made available sooner.
Executing the Analytics Agenda varies across organizations, since resources and partner collaborations are considerably different. The HDMS team fills in where needed and supports you on your terms. You might be almost self-sufficient, or you may want day to day help with general and deep-dive expertise for complex data analysis. Regardless of the resourcing model, through our technology your internal stakeholders and trusted business advisors will have relevant and progressive data analytics that enable intelligent decision-making.
A successful implementation is a given. Yes of course you’ll see value in phase 1. The Analytics Agenda reveals its “varsity” status as time moves on and you and your team just keep bringing the answers. Once the basics are taken care of, you will be able to move in so many directions, and your ability to serve your organization will create an acceleration effect.
The needs of employees and their families will change and so will the health care services they use, the programs offered, and the data produced and available to augment analysis. Bringing in new data sources and adjusting and adapting at the speed of change is a reality with HDMS. We work with you to understand your needs, create a plan, and execute at an accelerated pace. Our team and technology make it easy, and your Analytics Agenda means you know how and when you’ll deliver results – again and again and again.



March 11th saw the World Health Organization (WHO) declare a pandemic. This marked a change that immediately impacted our daily lives – our world has a new normal. In it, we need to rapidly adapt to change and healthcare data can show us what to tackle first.

Our ability to understand risk and anticipate spread of the novel coronavirus was inextricably linked to rapidly evolving data. What we understood and how we worked and played changed swiftly. Businesses that adapted quickly flourished while others failed.
Now more than ever, we need to harness health analytics to guide companies through ongoing data-driven decisions. We need to use data to plan for a continuously changing world.

HDMS recognized the opportunity to leverage our clinical and analytic experts to offer content to support companies that extend even beyond our own client base. We created an Analytics Agenda and shared supporting resources to best leverage health analytics to support your organization.
We recommended a framework of COVID-19 analytics that included these key focus areas in three phases:
Acute: quantify your population vulnerabilities for strategic planning and resource management
Short term: understand COVID costs, quantify cost offsets due to delayed or reduced care. Use this to re-plan the current benefit year, track wellness issues, and perform cost modeling for 2021
New normal: use COVID insights to tune benefit plans for 2022, manage wellness in our new world, accelerate good health and prevention
Now we’re in a new normal, and it only means transformation, innovation, and more change. Adjusting to this new normal, our clinical and analytic expert resources have been digging into the following areas. We’re building new client-specific reports, and rolling out new content in Enlight. What’s hot?
Leading indicators, trend stabilization, Mental health impact on chronic condition costs
Risk assessment and engagement strategies to offset foregone care
Billing inconsistencies (virtual care and telemedicine billing practices)
Care inequity baselines, Maternity & Fertility benefits, Transgender health
LinkedIn Article: Data tells a hopeful story of COVID-19 | Read
Five Tips for Optimizing your COVID-19 Cost Model | Read
LinkedIn Article: A helping hand – COVID-19 impact calculator | Read
Impact Calculator | Download
Countering COVID-19: Phased analytics shape benefits plans | Read
